Survival Mode
An Emory team in Madagascar tracks how germs jump between people and animals, hoping to help an ecosystem in crisis

Sarah Zohdy
“I smell props,” says Sarah Zohdy.
She looks skyward, scanning a tangle of thick, Tarzan-worthy vines, tree branches, and leaves that weave the dense rain forest canopy one hundred feet above.
“Do you smell that?” Zohdy asks a new arrival to Madagascar’s Ranomafana National Park. “They have a scent like maple syrup.”
Then, whoosh! A wide-eyed, fur-covered acrobat, mostly arms, legs, and tail, leaps out of one clump of leaves and disappears into another.
“Props!” Zohdy confirms, smiling at the comical performance of the creature. “Their legs are crazy long for their bodies.”
Propithecus edwardsi, more commonly known as a sifaka, is one of nearly one hundred species of lemurs. These primitive primates, with large, round eyes and wet, dog-like noses, are unique to Madagascar, an island in the Indian Ocean, off the southeast coast of Africa.
Lemur ancestors arrived in Madagascar some sixty-five million years ago, perhaps floating over from mainland Africa on mats of vegetation. Isolated on the island, the Earth’s fourth largest, lemurs evolved independently from other primates, diverging into a striking cast of characters: From the teddy-bear cute black-and-white ruffed lemur to the creepy, bat-like aye-aye.
Zohdy’s favorite is the mouse lemur, the smallest primate in the world. “The adults weigh about as much as a fun-sized package of M&M’s and can fit into the palm of your hand,” she says. “The babies are no bigger than a Ping-Pong ball and, basically, all eyeballs.”

"To really understand human health, animal health, and environmental health, you have to study all three at once," says Sarah Zohdy.
Carol Clark

A Malagasy village set on the edge of the rain forest
Kristin Derfus
A biologist in Emory’s Department of Environmental Sciences and the Rollins School of Public Health, Zohdy has been researching lemurs in Madagascar for seven years. Last summer, she broadened her focus and joined an Emory field team of infectious disease researchers, made up of students from a range of specialties, in Ranomafana. The Emory team is gathering baseline data for an ambitious “one health” intervention aiming to bolster the health of the rural poor around Ranomafana, who are struggling to stay fed, sheltered, and alive, while also conserving the ecosystem of the World Heritage site.
Zohdy’s rubber boots make loud sucking sounds as she trudges through thick mud toward a wooden suspension bridge spanning the Namorona River, roaring and rushing over its rocky bed even during the dry season. “Check out that spider web,” she says as she leads the way across the bridge. She points up at gossamer threads hanging above the water, leading out of the forest on one side of the river and stretching forty feet to connect with the trees on the opposite bank. The recently discovered Darwin’s bark spider, she notes, spins the largest webs in the world, and its silk is the toughest biological material ever studied—more than ten times hardier than Kevlar.

The clown-like face of a jewel-colored chameleon.
Sarah Zohdy
Crested drongos—large black birds sporting what look like elegant coattails and fancy feather headdresses—chatter in the trees alongside the slick forest trail, which is now leading steeply up a lush hillside.
Zohdy pauses when she hears breaking leaves in the canopy and catches a whiff of a musky, zoo-like smell.
“Golden bamboo lemurs. They are right above us,” she says softly.
“Don’t open your mouth when you look up,” she quickly adds. “People have been peed on.”
The dusky-gold creatures, which look like a cross between a koala bear and a raccoon, are critically endangered. They are one of three species of lemurs in the park that subsist almost entirely on the tender leaves and shoots of bamboo.
The greater bamboo lemur is the rarest of them all. Just two remain in the 160-square-mile Ranomafana National Park—a father and his daughter—and only about sixty survive in the wild.
Like the giant panda, the greater bamboo lemur has molars capable of slicing and crushing the tough trunk of bamboo. “It’s a fascinating evolutionary adaptation,” Zohdy says, that allows them to survive during the dry season, when the more tender bamboo shoots and leaves are not readily available. Loss of habitat and shifts in climate, however, have lengthened the dry season.
“That means the greater bamboo lemurs have to chew on the tough trunks longer, which wears down their teeth,” Zohdy says. “When their teeth go bad, they starve. It’s not like they can go to a bamboo lemur dentist and get dentures.”
Since humans began settling on the island about two thousand years ago, bringing a rice-growing culture with them, much of its natural habitat and wildlife have disappeared, including at least seventeen species of lemurs.

Propithecus edwardsi, more commonly known as a sifaka, is one of twelve species of lemurs found in Ranomafana National Park.
Konrad Wothe/Minden Pictures/National Geographic Creative
“When I first came to Madagascar, I thought the whole island would look like a BBC nature special,” Zohdy recalls. Instead, she was stunned during the ten-hour drive from the capital of Antananarivo to Ranomafana to see a largely treeless landscape of terraced rice paddies and occasional smoke from slash-and-burn agriculture.
“I just wanted to study aging in mouse lemurs,” Zohdy says. “I didn’t go into this wanting to be a conservation biologist, but I realized that was necessary.”
In the steep landscape of Ranomafana, the homes of villagers and their food crops and livestock bump up against the remaining patches of primordial wilderness. The crowding puts both people and animals at risk. “When you have humans encroaching on wildlife habitat, you have huge potential for zoonotic diseases, and the emergence of new diseases,” Zohdy says. Pneumonic plague and virulent strains of flu are examples of deadly outbreaks that have occurred in Madagascar in recent years.
The “one health” approach of the Emory infectious disease team may be key to solving some of the complex problems facing the Malagasy people and the fragile Ranomafana ecosystem.
Each summer since 2011, Emory student researchers have collected fecal samples of lemurs, people, and their livestock. These samples, along with mosquitos and ticks the team also collects, are sent back to Atlanta for analysis of pathogens they may contain.
The project is part of a large-scale conservation and global health effort being led by Thomas Gillespie, professor of environmental sciences and environmental health.

Chickens, horned zebu, and people share the same space in villages.

The Emory researchers found that a form of parasite that is usually associated with pigs is showing up in people.
Cassidy Rist
The fieldwork is not easy. It requires team members to camp out and hike up and down the steep trails of the region, often slogging through rain and mud, forging on even while occasionally suffering from bouts of the intestinal diseases they are there to investigate.
“One minute you’ll be struggling up a steep path, brushing back vines with thorns that tear at your hands,” says Zohdy, a postdoctoral fellow in the Gillespie lab. “But then you’ll round a corner and see a beautiful waterfall. Or you’ll look down at your boots and notice that the mud caking them is sparkling with flecks of gold.”
The data the students are gathering will help guide a health care improvement effort through a new nonprofit agency called PIVOT. The students on the 2013 team brought a breadth of experience and interests to the project, coming from Emory’s Department of Environmental Sciences, the Rollins School of Public Health, the Nell Hodgson Woodruff School of Nursing, and the Master of Development Practice (MDP) program. The work conducted last summer was largely funded by the Jim and Robin Herrnstein Foundation and Emory’s MDP program and Global Health Institute.
Emily Headrick 15N 15MSN is a nurse whose passion for global public health spurs her to choose fieldwork over hospitals.
“Madagascar is famous for its wildlife, to the point that its people get overshadowed,” she says. “When people’s children are dying of diarrheal diseases, their priorities are probably not going to include protecting biodiversity.”
She conducted health assessments of families that were randomly selected from the villages in the study. Few people she has surveyed own shoes or toothbrushes. One family, for example, consists of thirteen people living in a ten-by-two-foot mud-brick home with a thatched roof, a dirt floor, and little else.
In addition to asking questions about the health history of family members, Headrick’s role was to measure and record people’s height and weight and other vital signs and to test their blood for malaria. Most people have never been to a dentist, and some report debilitating tooth pain.
“I worked really hard to prepare myself for the fact that we are here to do research, and not to provide health care,” Headrick says.
Determined to do what she could, however, she bought drugs to treat anyone who tests positive for malaria. She also put together a comprehensive first-aid kit and spent much of her free time cleaning and bandaging wounds.
The simple act of touching someone and taking the time to listen to them talk about their pain is part of the role of a nurse, Headrick says. “It has a different kind of therapeutic value. And it helps build trust in people. This is a long-term project.”

Emily Headrick assesses the health of a young villager.
Carol Clark
Cassidy Rist 14MPH is a veterinarian who also works part time in the One Health office of the Centers for Disease Control and Prevention (CDC).
Rist interviewed people in village households about the animals they own, mainly poultry, pigs, and zebu—a hardy, humpbacked breed of cattle. In a typical village, ducks, chickens, zebu, and pigs wander amid the mud houses, defecating near water sources and on the same paths where people walk barefooted. People often cage their free-roaming chickens and bring them inside the family home to sleep at night.
“Any pathogens these animals have can easily be shared by the whole village,” Rist says.
Some people told her that their chickens died of malaria. She explained to them that chickens don’t get malaria. She then asked the symptoms of the birds, so she could give them information about the likely culprit.
Dogs are also in the mix, often scruffy with ribs showing, and rarely vaccinated for rabies. Rist asked if she could treat the badly injured paw of one dog. The villagers told her that it was fady, or taboo, to restrain a dog, so she was unable to help the animal.
Too many public health programs leave pets and livestock out of the equation, Rist says. “We need more projects like this, where people from different specialties work together and talk to each other.”

Cassidy Rist gathered data on livestock, including the most valuable animal of all to villagers—the zebu.
Carol Clark
“Studying diseases in a lab or a classroom is a lot different than seeing people affected by them in real life,” says Kristin Derfus 15MPH. “No one should be dying from these diseases. They’re treatable.”
In each of the villages of the Madagascar study, Derfus collected ticks and mosquitoes that were sent to the CDC for analysis. Cumbersome light traps, with lots of working parts, are used to capture the mosquitoes.
“A lot of things go wrong when you’re working in the field. I’ve learned to think creatively,” Derfus says. She was using plastic bags to keep the batteries of the light traps dry, but the bags leaked where the wires connecting them to the trap protruded. Zohdy grabbed a large banana leaf, slit it up the middle, and fitted it over the batteries. “The leaves work perfectly,” Derfus says.

Kristin Derfus used mosquito traps to identify "hot spots" where malaria-infected mosquitoes are the most abundant. Her data will help in the development of targeted interventions.
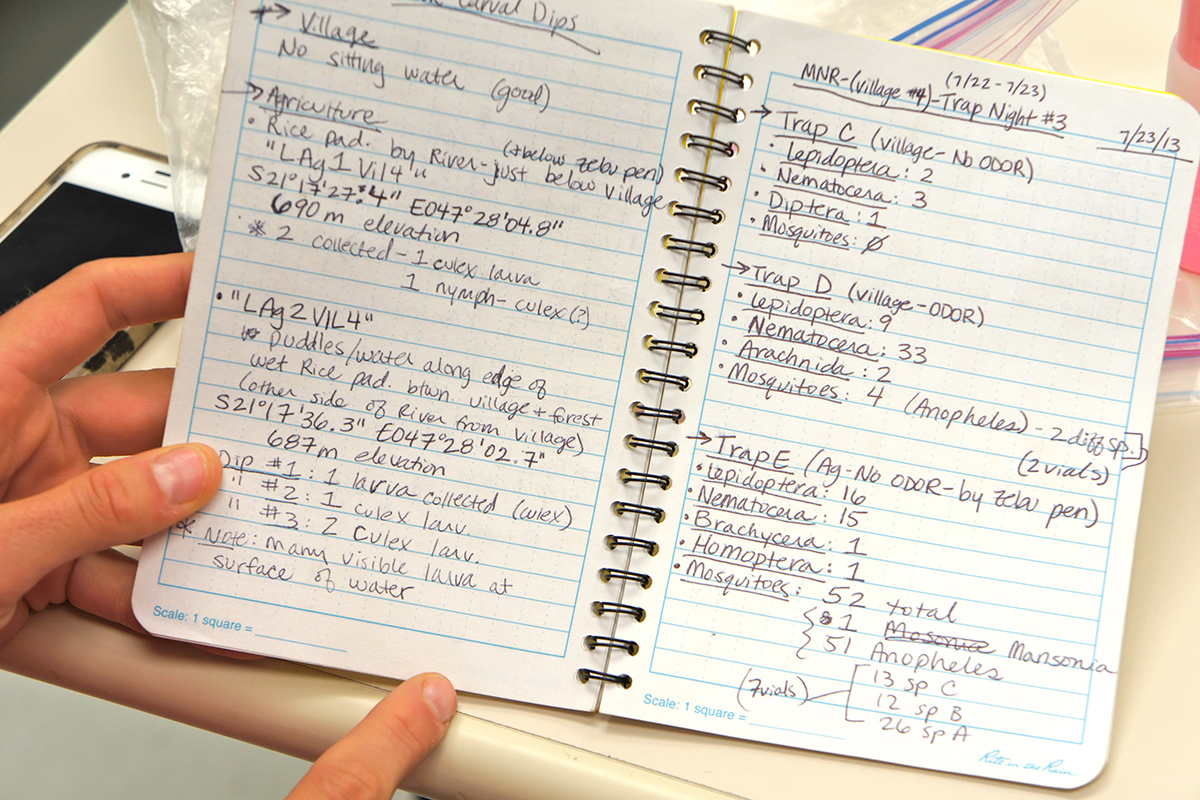
Derfus was rarely without her field notebook, where she recorded types of mosquitoes found and whether they were captured near homes, livestock pens, agricultural sites, or nearby forest.

"Malaria is a big, big problem in Madagascar," says Tovo Mbolatiana Andrianjafy, a Malagasy graduate student of medical entomology who worked with the Emory team in the field.
Carol Clark
Morgan Mercer 15MDP and Paul Kennedy 15MDP used GPS technology to survey the villages and their agricultural sites.
“We are mapping the layout and including water sources, latrines, livestock enclosures, streams, and roads,” Mercer explains. They will then add the GPS coordinates and data gathered by other team members on households, livestock, and surrounding forest, and any pathogens detected through analyses. The result will be a collection of data visualizations that can be viewed individually, or layered atop one another.
Ultimately, the project will not be successful unless it also considers the villagers’ complex views about their environment, Mercer says. “The Malagasy farmers work their land, feed themselves from it, feel tied to it, and ultimately should be the ones who have say over how it is managed.”
Kennedy served in the Peace Corps in Jamaica and earned a degree in nursing before entering Emory’s MDP program. He finds the Malagasy people exceptionally kind and is fascinated by their culture.
“I get bored watching lemurs after about a minute-and-a-half,” he says. “I appreciate the beauty of the environment, and it’s definitely a key component to this project, but I’m more into the people. It’s important that our data don’t just end up as statistics in a report.”

"I want to help deliver a tangible benefit to these villages," says Morgan Mercer, right, working in the field with local guide and technician Rakotonjatovo Justin.

Paul Kennedy spent his downtime from fieldwork on odd jobs like improvising an extra mosquito trap or repairing a village child's homemade top. "I like tinkering with things and building things," he says.
Carol Clark
Environmental sciences major Caroline Schwaner 14C says her favorite professor is Eloise Carter, a biologist at Oxford College who is well known for her class field trips to the streams and woods of Georgia.
In Madagascar, Schwaner used a net to scoop out invertebrates—insects, worms, and snails—both upstream and downstream from villages and agricultural sites. That gave her a glimpse into the water quality of streams used for drinking, washing, and bathing.
“Certain bugs are usually found only in cleaner water, and others thrive more in pollution,” Schwaner explains. Caddis fly larvae, for example, are indicators of clean water while beetles tolerate dirtier conditions.
Schwaner also used rapid detection tests in the field to screen human fecal samples for adenoviruses and rotavirus, two common causes of diarrhea. Back in Atlanta, she analyzed the fecal samples from humans, lemurs, and livestock for a broader range of pathogens.
Madagascar was Schwaner’s first experience in the developing world, and she admitted to culture shock. “One of the hardest things for me was getting used to using a latrine shared by a whole village,” she says.
The benefits far outweighed that inconvenience, she adds. “One day we saw four species of lemurs, just while we were walking to work.”

"I'm learning a lot about how to develop research methods in the field," says Caroline Schwaner, who used low-tech methods to gauge the water quality of streams running through villages.

Caroline Schwaner uses rapid detection tests to screen fecal samples for viruses.
Carol Clark
One evening, Zohdy leads students on the team on a night hike up the side of a mountain. The forest is eerily silent. A thick mist snakes along the ground and drifts up through the silhouettes of trees.
The researchers’ headlamps slice like lasers across the understory, occasionally striking treasure. An iridescent green and blue chameleon looks like a jeweled dragon clinging to the branch of a sapling. A golden moth the size of a small bird fans its wings across a clump of eucalyptus leaves.
“Do you hear that high-pitched trill, like a tiny, far-away bell?” Zohdy asks. “That’s a mouse lemur.”
Tiny pairs of glowing eyes pop out of the darkness. Mouse lemurs are nocturnal, and their eyes shine due to the reflective effects of sensitive night vision. The eyes appear, then vanish in a flash, as the shy creatures dart amid the branches of small trees.
Zohdy instructs everyone to switch their headlamps from white light to red, so the lemurs don’t get blinded.
Seen in well-lit photographs, the brown mouse lemurs populating Ranomafana are charming. They have a beguiling gaze and tiny, elegant hands that look more human than animal, complete with delicate fingernails.
Moving through the dark forest, however, these miniature primates become like lemures, Latin for ghosts and the origin of the word lemurs. They flit through the trees alongside the trail, watching the humans with wide, curious eyes that reflect the red glow of the curious humans staring back.

Brown mouse lemurs are tiny, nocturnal primates that populate Ranomafana and sometimes cross paths with people and livestock.
Frank Vassen/Wikipedia
Madagascar is an evolutionary biologist’s nirvana and worst nightmare. Most of the flora and fauna of the island, located off the southeast coast of Africa, is found nowhere else on Earth. But this unique ecosystem is critically endangered. About 90 percent of Madagascar’s original forests are gone, mostly due to slash-and-burn agriculture. Time is running out for many animals, including several species of lemurs that are near extinction.
Meanwhile, much of the human population is focused on staying fed, sheltered, and alive. The country is the fifth poorest in the world, with an annual per capita income of $400. About 160 children a day die in Madagascar from preventable diseases, according to UNICEF.
“Madagascar could be a poster child for the effects of environmental degradation and the lack of a viable public health care system,” says Thomas Gillespie, a disease ecologist and Emory professor of environmental sciences and environmental health.
“Globally, we are going to have to deal with the issues of climate change, growing populations, and dwindling resources,” he adds. “Madagascar is just an extreme example.”
Gillespie is director of infectious disease research and a board member of Centre ValBio, an international research consortium at the entrance of Madagascar’s Ranomafana National Park.
For the past three summers, Gillespie has sent teams of Emory student researchers to Ranomafana to gather baseline data on the health of people, domesticated animals, and wildlife in and around the park.
Analyses of diagnostic samples from humans, livestock, and wildlife—along with survey, observational, and spatial data—show how viral, bacterial, and parasitic pathogens are moving between all three. Some lemurs near villages have picked up the bacterium that causes cholera, for example, while a form of the parasitic diarrheal agent Cryptosporidium usually associated with pigs is showing up in people.
Zoonoses, or pathogens that move between animals and humans, sometimes morphing into deadlier forms, can spark pandemics and decimate populations of animals and people. “For the poor, acute and chronic diseases can create a negative downward spiral into a poverty trap,” Gillespie says.
The project is part of a large-scale, “one health” intervention to promote human and wildlife health, while ensuring ecological sustainability. In January, the nonprofit organization PIVOT launched a large-scale health improvement program in Ramomafana aimed at creating a system of universal access to quality health care in the region that will eventually serve as a model for the rest of the country.
PIVOT’s program will be guided by the Emory infectious disease team’s work to identify the area’s key pathogens and how they are transmitted, says Gillespie, who is on PIVOT’s board of directors. Harvard economist and disease ecologist Matt Bonds is executive director, and Michael Rich, a founding director for Partners in Health Rwanda, is the senior clinical adviser.
The team recently received a Grand Challenges Grant from the Bill and Melinda Gates Foundation and will use the award to develop the first combined standard measure of the economic burden of human and livestock diseases.
“This is a rare opportunity to determine if the theory that people can be released from the poverty trap through improved health care is a reality,” Gillespie says. “We will be looking at whether the PIVOT health intervention leads to less degradation of resources and an improvement in quality of life for the people of Ranomafana.”


