|
BY
MARY J. LOFTUS
Norris
Lake, about twenty miles east of Atlanta, is the first scheduled
pit stop for twenty riders taking part in this year’s ActionCycling
200. Each May, the riders pedal from Atlanta to Athens and back
again to raise money for AIDS vaccine research at Emory.
“The
butterflies, we call ’em,” says a local, who is manning
a table for the Norris Lake Neighborhood Association. “They
come flocking through here every spring in red, yellow, and
green.”
Harriet
Robinson, Asa Griggs Candler Professor and chief of Emory’s
Division of Microbiology and Immunology, has come out this Saturday
morning to cheer on the riders. She stands in the Phillips gas
station parking lot, eagerly scanning the horizon.
“Here
they are!” she says, spotting the front-runners in their
Day-Glo orange biking jerseys, helmets, and padded black shorts.
The first arrivals pull into the lot just after 9 a.m. and descend
on the support van to grab Powerade, pretzels, apples, candy
bars, and bananas.
 Robinson,
dressed casually in a sleeveless white top and blue slacks,
circulates among them, joking and making conversation. She is
accompanied by her four-year-old grandson, Jack, who is visiting
from Pittsburgh with his parents and younger brother, Gus. Robinson,
dressed casually in a sleeveless white top and blue slacks,
circulates among them, joking and making conversation. She is
accompanied by her four-year-old grandson, Jack, who is visiting
from Pittsburgh with his parents and younger brother, Gus.
“Do
you want to finish the ride instead of me?” a rider asks
Jack, noticing him admiring the sleek racing bikes.
The
group’s de facto leader, John Beal, organized Action Cycling
of Atlanta (motto: “pedaling for a purpose”) and has
ridden in races in Alaska, Canada, and across Montana that raised
millions of dollars for AIDS research.
“Basically,
a bunch of Atlanta riders did a European ride a few years ago,
and so little of the money went to where it was supposed to
that we resolved to start a ride here and make sure the money
went to the right place,” Beal says. The group raised $65,000
for the Vaccine Research Center last year and an additional
$20,000 so far this year.
Robinson
is a celebrity of sorts to this group. “Most of the bikers
know Harriet,” Beal says. “She’s the scientist
from Emory who has an AIDS vaccine in clinical trials. She came
to Athens last year and talked to us. She’s probably not
as well known as she will be one day.”
By
9:30 a.m., almost all the cyclists have checked in, reenergized,
and are ready to start out for Walnut Grove, the next stop.
Two riders, though, haven’t shown up yet. A few minutes
later, they pull in together– Michele Hennessy, who went
an extra four miles after missing a turn-off sign, and Joy Martin,
who looks flushed but elated.
“I’ve
never ridden this far in my life,” Martin announces.
“Well,
I tell you, you are courageous,” Robinson replies.
The
same may well be said of the sixty-six-year-old Robinson, a
top researcher at Emory’s Vaccine Research Center who–through
sheer tenacity and despite a number of obstacles that might
have discouraged those with less gumption–has developed
one of the most promising AIDS vaccines in clinical trials today.
For
much of her career, Robinson was a single mother of three boys,
the sole woman in a roomful of male scientists (“They would
call the men ‘Dr. so-and-so,’ and I would just be
‘Harriet,’ ”) and an independent thinker who
often fell outside of the scientific mainstream.
Her
early successes in using DNA to create vaccines were met with
skepticism–professional journals wouldn’t publish
her results and her grant proposals were routinely refused.
“You don’t think this will ever be useful, do you?”
read one reviewer’s comment.
Still,
Robinson has taken her groundbreaking DNA-based AIDS vaccine
from the lab through successful primate trials and into human
testing–even when she’s had to brave machine-gun fire
during rebel insurrections to do so.
“I
believe our vaccine has real potential,” Robinson says.
“There is a subset of the research community that is discouraged.
They criticize us for being overly optimistic. But the fact
remains that our vaccine works in monkeys.”
After
years of combatting the naysayers, Robinson’s life runs
fairly smoothly these days–her research is well funded,
she is highly regarded as a scientist, and she lives quietly
in a modest brick ranch on a wooded lot near the Emory campus,
a short drive from her lab at the Yerkes National Primate Research
Center.
“We
used to walk our dogs together in the mornings,” says Tom
Insel, former director of Yerkes who is now head of the National
Institute of Mental Health, “and the great thing about
Harriet is that she was always thinking about science–how
to get the next project completed, what the most recent results
might mean, where to get the best advice. Her concerns were
never about personal gain or recognition. I have never known
a scientist with so much talent and so little ego.”
The
virus Robinson is squaring off against is the most lethal infectious
disease in the world: AIDS has killed twenty-two million people
globally since 1981, and forty million are currently infected.
In the United States, more than one million have the virus; in
China and India, more than ten million are infected in each country,
as are an estimated 30 to 60 percent of the sub-Saharan population
in Africa.
And
the spread continues. Almost five million people were infected
last year, the largest number of new cases since AIDS was discovered,
and three million died. Young people fifteen to twenty-four
years old account for nearly half of all new infections worldwide.
Sixty-eight million people are projected to die from AIDS by
2020–more than the entire population of Great Britain.
The
scientist who develops an affordable, effective AIDS vaccine
will save more lives than have ever before been spared by a
single medical innovation save, perhaps, the discovery of penicillin.
“AIDS
is an extraordinary kind of crisis; it is both an emergency
and a long-term development issue,” states the 2004 United
Nations AIDS Report on the global epidemic. “Despite increased
funding, political commitment, and progress in expanding access
to HIV treatment, the AIDS epidemic continues to outpace the
global response. No region of the world has been spared. The
epidemic remains extremely dynamic, growing and changing character
as the virus exploits new opportunities for transmission.”
By
now, the devastatingly effective strategy of the AIDS virus
is well known: the virus invades the human immune system, targeting
helper T-cells and macrophages–the very white blood cells
sent to destroy it. Opportunistic infections and cancers that
the body could normally fight off quite easily ravage people
with AIDS, once their immune systems start shutting down.
No
successful treatment for AIDS existed until 1987, when the first
antiretroviral drug was discovered. Antiretrovirals, which work
by slowing the reproduction of the virus, are now given in combinations
(anti-HIV “cocktails”) that can reduce death rates
by more than 80 percent.
But
such drug regimes, which must be taken consistently and for
life, are expensive–from $12,000 to $45,000 a year per
person–and the vast majority of those with the virus live
in developing countries where such costly treatments are not
an option.
Researchers
also worry that widespread misuse of anti-HIV drugs by patients
who take them only sporadically, compounded by haphazard manufacturing
practices in labs that don’t meet rigorous standards, could
spawn future epidemics of drug-resistant strains of the virus.
“The
real solution for the world,” says Robinson, “is a
vaccine.”
Vaccines
prime the immune system to recognize disease-causing organisms–similar
to providing a mug shot (“Look out for this guy, he’s
dangerous”) so that the body’s defenses will spring
into action when they encounter the virus.
The
impact of vaccines on public health over the last century has
been substantial: smallpox has been eradicated, polio has been
greatly reduced, and cases of measles and Hib (haemophilus influenzae
type b, at one time the leading cause of childhood bacterial
meningitis and mental retardation) are at a record low.
But
developing a vaccine for AIDS is especially difficult, says
Rafi Ahmed, director of Emory’s Vaccine Research Center,
because the virus is constantly changing and mutating. “HIV
presents a moving target, essentially,” says Ahmed. “You
have to understand both the virus and the immune system to develop
an effective vaccine.”
Traditional
vaccines are made from the virus itself, which has been killed
or weakened. The danger is that such a vaccine, if not properly
inactivated, might actually induce the illness; the original
version of Jonas Salk’s polio vaccine caused two hundred
and sixty cases of the disease, resulting in ten deaths.
But
Robinson’s vaccine, developed in collaboration with the
National Institutes of Health (NIH) and the Centers for Disease
Control and Prevention (CDC), is unique in that it is a DNA-based
vaccine–a technique Robinson pioneered. DNA vaccines stimulate
an immune response by using only pieces of the virus instead
of the virus itself, so the recipient is never placed at risk
of infection.
Robinson’s
AIDS vaccine requires three shots: a DNA-based inoculation to
prime the immune system, followed by two poxvirus booster shots,
which increase the body’s immune response. “The DNA
vaccine establishes the breadth of the immune response,”
she says, “while the poxvirus boosters affect the height
of the response. The result is that the combination is more
effective than either one alone.”
Robinson
chose poxvirus, a version of the virus first used as a smallpox
vaccine, for the booster because it was large enough to carry
several extra HIV genes.
“The
pox viruses are enormous,” she says. “They are like
the Battleship Galactica of viruses.”
Robinson’s
vaccine has tested well in trials with rhesus macaque monkeys
at Yerkes. Twenty-three of twenty-four monkeys given the DNA
vaccine and poxvirus booster failed to develop AIDS symptoms
even after exposure to high levels of the virus. In the control
group, five of six non-vaccinated monkeys died of AIDS within
six months of being infected with the virus.
“To
our knowledge, no other HIV vaccine or large-size trial, has
reported such a high level of protection for such a long period
of time,” Robinson says.
The
vaccine has been approved by the Food and Drug Administration
for human trials, which began in January of 2003. HIV-negative
volunteers were randomly assigned to receive one of the following:
high-dose vaccine, low-dose vaccine, or placebo.
“We’ve
had the DNA vaccine in clinical trials for a year and a half
at three different sites–Seattle, San Francisco, and Birmingham–in
thirty people,” Robinson says. “These trials have
been very successful in showing that the vaccine is safe for
humans.”
The
next series of human trials is scheduled for early 2005 to determine
the safety of the DNA prime combined with the poxvirus booster,
and to establish a dosing schedule. After this, a third series
of trials will be conducted in a population at high risk for
acquiring AIDS, with some volunteers receiving the vaccine and
others receiving a placebo, to gauge effectiveness.
Robinson
believes a usable AIDS vaccine is still five to seven years
away but, she adds, “I have great hopes.”
Giving
up isn’t in Robinson’s lexicon, says Helen Drake-Perrow,
her office manager of seven years. “She inherited from
her parents a sense of ‘can do’–working things
out for herself instead of relying on others. She is independent,
has clear logic, and is full of confidence, yet is still humble.”
Harriet
Latham Robinson was reared in Boston, the only girl among three
brothers. She remembers her mechanical engineer father, Allen
“Jack” Latham, tinkering in the basement with his
inventions. He was later named New England inventor of the year
for creating a disposable centrifuge to separate blood.
Her
mother, Ruth Latham, earned a master’s degree in chemistry
from Oberlin and taught organic chemistry at Smith College before
staying home to raise a family.
“She
would say sodium bicarbonate for baking soda, or H2O for water,”
Robinson recalls. “We were always doing interesting things.
As kids, we made tents and spent a lot of time outdoors. We
had an enormous garden. I think we were the last family in the
city of Boston to keep chickens.”
Despite
her mother telling her “an educated woman can never be
happy,” Robinson became a scientist–and an academic.
“I went to Swarthmore intending to major in history,”
she said, “but I became fascinated by the development of
organisms.” She went on to attend MIT, where she earned
a master’s degree in molecular biology and a Ph.D. in microbiology.
Receiving
her doctorate in 1965, a time when just 8 percent of science
Ph.D. graduates were women, didn’t faze Robinson. She loved
being one of the new recruits in the fledgling molecular biology
department at MIT and thrived on the synergistic environment
of the lab.
She
won a postdoctoral fellowship in the virus laboratory at the
University of California at Berkeley, where she met her husband,
William Robinson, who was also a scientist. They had three sons.
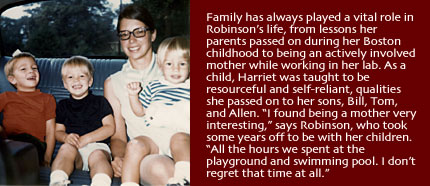
“I
basically became a full-time mother,” she says. “I
worked two mornings a week in a lab, but I found being a mother
very interesting. Some of my very best friends are from that
part of my life–all the hours we spent at the playground
and the swimming pool. I don’t regret that time at all.”
When
her sons were five, six, and seven, Robinson went through a
divorce and became a single mother.
“I
tried to get a job in California, but no one would hire me as
faculty or a technician,” she says. “So I looked all
over the country, and ended up back in Massachusetts, at the
Worcester Foundation [for Experimental Biology.] I had a lab,
and they had their new scientist.”
Robinson
stayed at the Worcester Foundation–famous as the lab where
“The Pill” was developed–for ten years. Her research
on viral-induced cancers led to the identification of host genes
that can be mutated by viruses into cancer-inducing genes. Robinson
also discovered that an immune response could be triggered if
viral DNA was injected into chickens.
“Harriet
became enchanted with the idea of using DNA itself as an immunizing
agent,” says Thoru Pedersen, professor of biochemistry
and molecular pharmacology at the University of Massachusetts
Medical School, who was Robinson’s colleague of many years
at the Worcester Foundation. “Harriet has absolutely fearless
courage to pursue new ideas. She’s willing to try things
off the beaten path, and through this, she has become quite
famous in the field of virology.”
While
Robinson worked nine to five, a live-in housekeeper managed
the homefront. But Robinson put in plenty of parenting time
herself. Colleagues remember that her license plate spelled
out, “HEY MOM.”
After
her sons left home one after the other to attend Stanford University,
where their father was a professor, Robinson began working more
hours in the lab. “I had the worst case of empty nest syndrome,”
she says.
In
1988, she was recruited to a research position in the pathology
department at the University of Massachusetts.
“Harriet
was working on a type of molecular pathology that was technically
very advanced, but conceptually very simple: since vaccine production
is essentially a matter of protein synthesis, the fastest way
to generate the specific protein is to teach the cell how to
make it by providing it with specific, ready-made DNA,”
says Guido Majno, then chair of the pathology department. “It
seemed so obvious and promising, why had it not been done before?”
Robinson
began developing a simian version of the AIDS vaccine. The thinking
in the scientific community at the time, though, was that DNA
vaccines would never work because the DNA would not be taken
up by enough cells to produce an immune response.
“No
journals would publish my results. My grants kept getting turned
down. My department chair actually used department funds to
keep me going at a critical point. But I didn’t abandon
it,” she says. “I always thought it would come through,
because the lab results were so good.”
By
1992, more scientists were working on DNA vaccines, which had
become more widely acceptable; Robinson’s results were
published in the Proceedings of the National Academy of Sciences
and in the journal Vaccine.
Now
Robinson was able to turn her attention more fully to developing
a human AIDS vaccine. The complexity of the virus itself fascinated
her: the way it killed the helper T-cells of the immune system,
its resistance to containment.
“If you vaccinate but you don’t protect the helper
cells, you’ve lost your supply lines.” she says. “It’s
like Napoleon’s army in Moscow after winter comes.”
Drawn
by the breeding colony of rhesus monkeys at Yerkes National Primate
Research Center–one of eight national primate research centers
funded by the National Institutes of Health (NIH)–Robinson
came to Emory in 1997 as chief of microbiology and immunology.
She joined a cadre of internationally known researchers working
on vaccines for diseases including malaria, herpes, hepatitis
C, and influenza.
“The
closest I’ve come to the MIT environment is the Vaccine
Research Center here,” says Robinson, “just in the
confluence of people and the excitement about what’s going
on.”
The
Vaccine Research Center at Yerkes was the perfect fit for another
reason as well: Developing an AIDS vaccine is the center’s
primary goal.
“Harriet
had a different strategy for approaching vaccine development,”
says Insel, the former director of Yerkes who recruited Robinson.
“All of the major companies had shut down their AIDS vaccine
programs and moved to developing retroviral drugs, so she was
already a bit of a maverick for committing to a vaccine. Her
DNA approach, which was revolutionary at that time, was really
intriguing because it represented a new way of thinking about
vaccines. DNA is heat stable, so if the vaccine was effective
it could be used in Africa or Asia without refrigeration–an
obvious plus for global health.”
In
2001, results from Robinson’s monkey trials were published
in the journal Science, with Yerkes Assistant Research Professor
Rama Amara as lead author. It became the most cited paper in
immunology for several months, and Robinson joined the elite
group of researchers at the front of the AIDS vaccine race.
Make
no mistake–for these scientists, this is the Tour de France,
and they want to win. There is cooperation, but there is quite
a bit of competition as well. Once a vaccine is available, the
demand will be abundant: market estimates are between four billion
to ten billion dollars per year.
Merck,
Chiron, Aventis-Pasteur, Glaxo-Smith Kline and the NIH Vaccine
Center are all working on AIDS vaccines, as are several other
universities, including Oxford, Yale, and the University of
North Carolina.
“In
a sense, the competition has been consciously generated by funding
agencies and the NIH,” says Neal Nathanson, vice provost
for research at the University of Pennsylvania and former director
of the Office of AIDS Research at NIH. “They put out enough
money to bring into the field anyone who has a credible idea.”
Robinson
believes that in the end, there may be more than one AIDS vaccine,
just as there is more than one polio vaccine. “Typically,
after a vaccine is developed in a lab, it is handed over to
a large pharmaceutical company for commercialization,”
she says. “But I really want to retain control through
the efficacy trials.”
These
days, work in the lab and with the monkeys is handled by lab assistants,
vet techs, and animal techs, rather than Robinson, who concentrates
on writing grant proposals and dealing with government regulations–the
frustrating logistics of birthing a vaccine.
Still,
her reserves of courage and tenacity are sometimes called upon.
In
the fall of 2002, Robinson flew to the Ivory Coast for a series
of meetings organized by the CDC and the health ministry about
testing a version of her vaccine in Africa. The plan was to
establish a vaccine clinic in Abdijan, the capital city.
At
her hotel, she awoke in the middle of the night to a sound like
a truck running into a wall and scattered machine-gun fire.
“I just stayed in bed through the whole thing,” she
says.
“I
don’t think any of us had any idea how bad it was,”
says Jeff Lennox, an Emory professor of infectious diseases
and director of the Ponce AIDS clinic, who was also in Abdijan
for the meeting. “When we got up the next morning, the
door to the hotel was shot out. We were told to stay inside.
You could see buildings burning, but there were no vehicles
moving outside. It was totally quiet.”
The
team was trapped in the hotel for two days. “Harriet was
great,” Lennox says. “Some people were very stressed
out, but she was very calm.”
They
were finally hustled into a van and taken to the airport, where
an Air France 747 touched down long enough to fill with Americans,
embassy workers, and airline staff. It was the one plane allowed
to leave the city.
“Harriet
was mostly upset that so much planning and organizing had gone
into this multi-country effort to have HIV trials in Africa,
and it wasn’t going to happen,” Lennox said.
Robinson
admits it was a great disappointment. “It was the perfect
place to do a trial. We lost so much to political instability,
it’s just tragic.”
But
the Ivory Coast setback seems only to have increased Robinson’s
determination to see her vaccine through to production and distribution.
Her team is now getting two vaccines ready for developing countries–one
for Africa and one for India–so that at least one will
make it through testing.
“We
still have very hard work ahead,” she says. “A lot
of critical junctures. We only go down in AIDS history if we
make it across the finish line.”
|