The Problem Solver
Porter Anderson was a tall, skinny towhead from Alabama who came to Emory in the fifties, won a Woodrow Wilson Fellowship, got a doctorate at Harvard, and went on to create a vaccine credited with saving the lives of 668,661 children—and counting.

Courtesy Porter Anderson
Porter Anderson 58C was a tall, skinny towhead from Alabama who came to Emory in the fifties, won a Woodrow Wilson Fellowship, got a doctorate at Harvard, and went on to create a vaccine credited with saving the lives of 668,661 children—and counting.
You probably wouldn't learn any of that if you talked to him, though. You'd have to Google Anderson to find out that in 1996 he and three colleagues were awarded the Albert Lasker Clinical Award, one of the highest honors in medical science.
Miami pediatrician Warren Quillian 58C was an Emory classmate of Anderson's who later worked with him at Boston Children's Hospital. "Whoever would have thought that this quiet, self-effacing guy would go on to become a giant—really, a giant—in the field of immunology?" Quillian says. "And as if it wasn't enough to invent vaccines for infant meningitis, he felt it was critical that a way be found to manufacture them inexpensively for children in the developing world, because the early versions were costly to make."
Anderson may be a cross between a polymath and a Renaissance man. Although he gravitated to science and enjoyed studying organic chemistry under Professor Leon Mandell, his happiest memories of Emory are the history classes he took with Professor George Cuttino, Shakespeare with Professor of English Roland Frye, and the "Athletics for All" sports program. Overcoming the handicap of a gimpy leg, he worked his way up to become an alternate on the Emory tennis team. And although he would deny musical ability, he still plays the Chopin mazurkas today that he did in college.
But there was a darker side to Anderson's Emory years. The mid-fifties—more than two decades before the Woodruff gift launched the University into the orbit of top-tier research institutions—were bringing great change to a nation awakening to the need for racial justice and equality. In some ways, the Emory he recalls, like most Southern schools, lagged behind leading universities in other parts of the country, both in education and in ethos. Anderson, on reflection, finds Emory's progress to be halting. "I could not understand how they had Brotherhood Week, and yet not one black student was enrolled in the College," he says. He also observed what he considered discrimination against Jewish students among the fraternities, a practice he thought the administration did little to address.
"When I came there as a seventeen-year-old, I didn't know much about the world, and Emory presented itself as a place where you were involved in success," Anderson says. "I took what was laid out for me as a matter of course. Only toward the end did I start to think of some of the negatives. I was in a fraternity, and I resigned from it because I came to think of it as waste of time and money, and an influence for bad conduct."
Anderson's strong feelings about the need for equality in education in the South later led him to spend two years teaching at the predominantly black Stillman College in Tuscaloosa, Alabama, from 1966 to 1968. "However, I disliked the Sisyphean quality of teaching, and preferred solving concrete problems," he says. From there he became a delegate to the famous 1968 Chicago Democratic Convention, as a member of an integrated splinter group from Alabama.
After graduating from Emory in 1958, Anderson spent three years as an agricultural chemist working on United Fruit's banana plantations in Honduras, where, he says, "I became skillful in lab work and aware of third-world health challenges." He later returned to the US and Harvard to earn an MA and PhD in bacteriology.
In 1968, a friend and colleague, pediatrician David Smith, sparked his interest in the bacterium known as Haemophilus influenzae type b, or Hib. The bacterium mainly affects children because they lack the natural antibodies to fight it, and typically causes meningitis, an infection of the covering of the brain and spinal cord. Each year some twenty thousand children in the US alone were being affected, and 5 percent died. While many in the industrialized world might recover, up to 45 percent were left with other problems such as deafness, brain damage, and epilepsy. In addition to childhood meningitis, the Hib bacterium also causes pneumonia, pericarditis, and arthritis.
Anderson and Smith partnered to set out on a near-epic twenty-year pursuit of a vaccine for Hib. As the self-described "bacteria juggler" of the two, Anderson spent thousands of intense hours in the lab working to perfect the vaccine by extracting and purifying the bacterium's outer slime layer—technically a molecular structure called a polysaccharide—while Smith worked to raise awareness and money. The pair tested early versions of their vaccine on themselves and colleagues before testing it on children.
There were breakthrough moments, certainly, but Anderson likens lab research to clocking in at a regular—if somewhat lonely—job. "I am something of a night owl, and I tended to arrive late and stay late, working by myself," he says. "For the most part it was just doing one thing after another, putting things into test tubes and watching them change color. But there were moments of suspense and excitement, particularly in getting samples from people who had been vaccinated to see if they had a response or not."
Clinical trials that administered the vaccine to 100,000 children in Finland in 1975 showed protection for toddlers, although not infants, whose immune systems are less developed. But the Finnish trial results served as a strong incentive for Anderson, Smith, and colleague Richard Insel to begin the little company that would become Lederle-Praxis Biologics (later acquired by Wyeth, now a major subsidiary of Pfizer). The strategy was to get licensure in the United States for the plain polysaccharide vaccine and to use revenue from this fund to develop the second-generation vaccine they hoped would protect infants (see sidebar).
"Our work was on a small scale," Anderson says. "To get into the field, the vaccines needed—and any new vaccine will need—major investment and skilled development by the vaccine industry and work by the FDA and the CDC to ascertain safety and actual disease prevention."
The first vaccine, for older children, was approved for use in 1986, and the second, for use with infants, was approved in 1990. Anderson and Smith's persistence has paid tremendous dividends, saving tens of thousands of young lives and preventing lifelong disability for many more.
This is the work for which Anderson, Smith, and NIH scientists John Robbins and Rachel Schneerson received the 1996 Albert Lasker Clinical Award. "Since conjugate vaccine was introduced," reads the Lasker Award citation, "Hib meningitis has been reduced by about 98 percent in the United States. The vaccine offers the hope that Hib-related diseases can be virtually eliminated."
Anderson was inducted into the National Academy of Sciences in 2010, and earlier this year was appointed as a fellow of the American Academy of Microbiology.
Asked how he feels about saving so many lives, Anderson says, "I rarely think about it. It was nice to have done, but I tend to think about what's ahead."
And the Lasker Award? "It opens a few doors when I am trying to get someone interested in a new project. Like the National Academy membership, it might get you a few moments of someone's time who would not ordinarily call you back."
Two Problems, Two Vaccines
Phase II: An early Hib vaccine developed by Porter Anderson and David Smith worked on toddlers, but not infants. Their immune systems are too immature to have the "memory" necessary to make the antibodies to fight bacteria; their cells, in essence, don't recognize the enemy.
Since most cases of Hib meningitis occurred in the first year of life, Anderson and Smith worked to develop a second-generation vaccine specifically for use in young infants: a "conjugate" vaccine, in which the purified polysaccharide is conjugated, or linked to a carrier protein. The carrier triggers T-cells (a type of white blood cell that recognizes foreign proteins) to mount an effective immune response.
Today, the Hib vaccine is recommended by the Centers for Disease Control and Prevention for all children under five, with more than 95 percent effectiveness. Prior to the vaccine, some twenty thousand US children contracted Hib-related meningitis annually, and 45 percent were left with permanent damage. Now cases have decreased by 98 percent.
Lure of the Lab
After the successful manufacture and distribution of the Hib vaccine in the US, Anderson was running a busy lab at the University of Rochester, raising money in addition to doing research. "I got very weary of that," he says. He decided to take a sabbatical and move to a home he bought on the Atlantic Ocean side of Key Largo in the Florida Keys.
But his mind continually wandered to vaccine development, specifically against pneumococcus. This bug is well-known as a cause of pneumonia in adults, but is more prevalent in infants, also causing meningitis. The World Health Organization (WHO) estimates that pneumococcus kills a million children each year, mainly in third-world settings.
In the 1990s, conjugate-type vaccines for pneumococcus were under development by several companies. These are inherently expensive because there are many different polysaccharide types that need to be included. WHO began to look for cheaper methods, and asked Anderson to join an advisory panel. He reviewed numerous proposals and began to have his own ideas about how to make a vaccine.
"He couldn't stay out of the lab for long," says Richard Malley, a pediatrician and infectious disease specialist at Boston Children's Hospital. As he had semiretired in 1996, Anderson needed a work site and basic research equipment—ultimately furnished by the hospital, where the two met. "One day I heard a crash from Porter's area, next door to mine," said Malley. "He had dropped a flask. We met as we mopped up the floor, and that was the beginning of a fifteen-year friendship. We started playing tennis together, and talked about developing this inexpensive way to make a pneumococcus vaccine. I knew that's what I wanted to do . . . to learn from this brilliant, quirky fellow. So he became my mentor."
Their approach includes the option to put the vaccine onto the mucous membranes of the nasal or oral cavity—similar to the flu mist commonly used now—both for the economy of omitting sterile injections and for the combination of internal and mucosal immunity that results.
The goal of developing an economical pneumococcus vaccine was to prevent disease in infants, but Anderson believes it will likely help susceptible adults as well, including AIDS patients and the elderly. The organization PATH funded the manufacture of the vaccine for human trials by the Butantan Institute of Sao Paolo, Brazil. The vaccine has not yet been approved for human testing in the US by the FDA; Anderson and Malley hope this will happen within the coming year.
Since his semiretirement, Anderson has been able to focus on the work he likes and leave the "paperwork" to others. "I never had much of a vision of what I would be doing, but I am very practically oriented and like to deal with concrete problems," he says. "In spirit, I'm a Yankee engineer more than a scientist. Real scientists look for problems to solve. I use whatever is at hand to solve a problem that is already there, to chip away at it."
Porter in Paradise
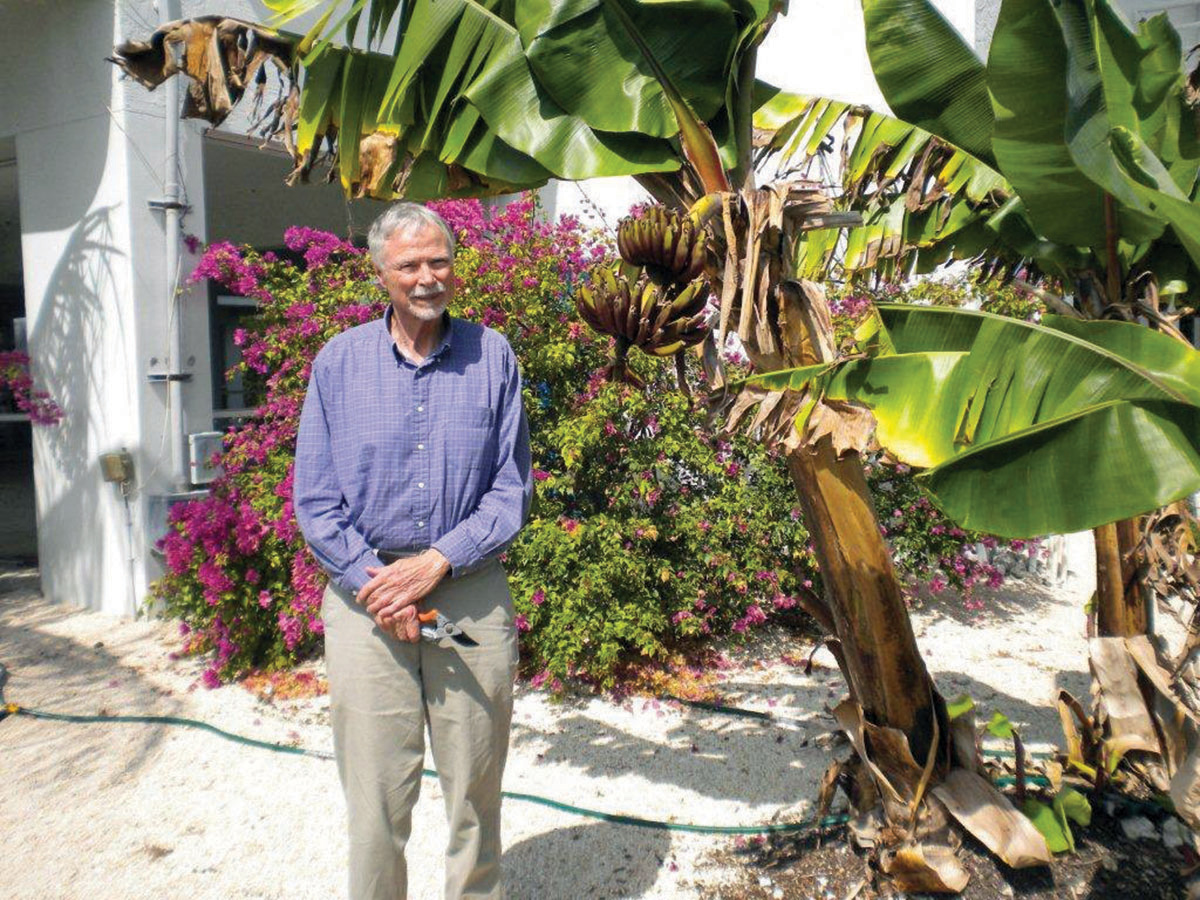
Easy Does It: Anderson relaxes at his home in the Florida Keys, but you'll only find him here about a third of the time, when he's not working on a vaccine.
David Pearson/Special
The two-story house where Anderson spends about a third of his time looks out over a canal and a mangrove-fringed bay toward Carysfort Light, just shy of the Gulf Stream.
All the living spaces and decks of the contemporary home are upstairs; below is a large carport where he keeps his tiny fleet of canoes, kayaks, and dinghies. They are light enough for two to carry, and it's only about a hundred yards to the ocean's edge and his launch site in the mangroves.
The house is the site of frequent gatherings of Anderson's eclectic coterie of friends (including several of his closest, friends since their days together at Emory). Besides his sister Sally, her son Andrew and his son Henry, her daughter Juliette and Juliette's husband Ralf, he might have friends down for morning canoeing, a lunch of shrimp salad and banana bread, and a concert on his grand piano given by a visiting pianist from the University of Miami. Or just as likely, a cabaret performance with one of his friends playing and singing "Brush Up Your Shakespeare," from Cole Porter's Kiss Me Kate. Until a recent hand injury forced him to the sidelines, Anderson also was the acknowledged tennis champion among his family and friends.
Harking back to his days on the plantations of Honduras, Anderson has planted several banana, key lime, mango, and coconut trees in the yard next to his house. His property fronts on an old canal whose brackish water is an ideal home for small landlocked tarpon; the house is set in the middle of a state-owned forest nature preserve.
Anderson's quiet life in the Keys is an hour from Miami and fifteen hundred miles from the bustle of Boston. His mind, though, is never far from the lab—at least, not while problems like pneumococcus still linger, unsolved.
David Pearson 58C lives in Florida and owns a strategic marketing firm for resorts. He was Anderson's dorm counselor in Dobbs Hall and has maintained his friendship through the years. Anecdotes from Moe's and Joe's bar have been edited out of this story.
Email the Editor