But
America’s greatest public health vulnerability–the
deteriorating condition of the country’s emergency healthcare
system–is being ignored, says Arthur Kellermann ’80M,
chair of emergency medicine for Emory’s School of Medicine.
“Despite
all the money that is going to homeland security, emergency
services has been elbowed out of the way. . . . This is where
the most critically injured would be taken. If we can’t
stay open, who’s going to provide the care?”
As
a doctor on the front lines at Grady Memorial Hospital’s
Emergency Care Center (ECC), Kellermann daily witnesses a system
pushed beyond the breaking point: harried nurses, patients lined
up in hallways, and overtaxed physicians who sometimes dread
going to work.
In response, he has become a national spokesperson on the issue
of emergency room gridlock, badgering congressional committees,
government agencies, and medical associations alike.
“E.R.s
are filled to the rafters with ill and injured patients because
inpatient beds are full or aren’t adequately staffed,”
Kellermann says, standing in the hallway of Grady’s ECC
as patients on stretchers are wheeled past. “So the patients
are trapped like soldiers on Omaha Beach: They can get in the
E.R. door, but they can’t advance any farther into the
hospital.”
Ninety
percent of hospitals across the country report that they are
operating at or above capacity, according to a survey by the
American Hospital Association. On any given day in metro Atlanta,
several major hospitals may be on ambulance “diversion”
at one time, meaning that their emergency departments are so
overcrowded that ambulances must go elsewhere.
“Right
now, Atlanta area hospitals couldn’t handle an airplane
crash, let alone thousands of casualties from a terrorism incident,”
says Kellermann.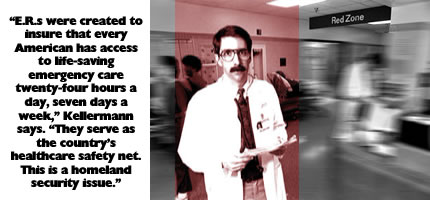 Nationwide,
emergency room visits increased by five million in 2001 and
are still on the rise–due to aging, population increases,
and a growing number of uninsured. One in six Americans now
lacks health insurance. Medicare patients are being dropped
by their primary-care physicians due to decreasing reimbursements.
Nationwide,
emergency room visits increased by five million in 2001 and
are still on the rise–due to aging, population increases,
and a growing number of uninsured. One in six Americans now
lacks health insurance. Medicare patients are being dropped
by their primary-care physicians due to decreasing reimbursements.
Because
E.R.s must accept patients, they have become providers of health
care for millions who have nowhere else to go. “In emergency
departments, we keep redefining the limits of what’s acceptable,”
Kellermann says. “Every day it gets a little worse. Administrators
think E.R.s are the only infinitely expansible space in the
hospital. Somehow, we find a way to stagger through the shift
no matter how bad it gets. But there are near misses in all
the chaos and flurry that the public isn’t aware of. It’s
like two commercial planes that fly less than a hundred yards
from each other–only the air traffic controller knows how
close it was. That happens all the time in America’s E.R.s.”
Grady,
Atlanta’s public hospital and only level one trauma center–and
a principal training ground for Emory physicians–has seen
a 15 percent increase in uninsured patients since last year.
This represents an additional burden of $15 million. “We
cannot continue to do more with less,” says Karen Frashier,
vice president of public affairs at Grady.
“This
is a problem that is threatening access to lifesaving emergency
care,” Kellermann says. “In the best of times, this
should be deeply disturbing. Now that our nation is engaged
in a war on terrorism, it is unconscionable.”
Emory
has one of the country’s oldest and largest residency programs
in the specialty of emergency medicine. Many of its graduates
go on to staff hospital emergency departments throughout Georgia
and the country.
“Emergency
medicine specialists are highly regarded for their ability to
think clearly and act quickly to save lives,” says Kellermann,
who oversees the emergency departments at Emory, Crawford Long,
and Grady. “We are also big believers in prevention, because
we see what happens when prevention fails.”
Kellermann
has long made it a practice to take on daunting problems that
threaten the common good. A 1980 graduate of the Emory School
of Medicine, he holds a master’s degree in public health
from the University of Washington. He returned to Emory in 1993
to found and direct the Center for Injury Control, which combines
the strategies of prevention, acute care, and rehabilitation
to reduce the impact of accidents and injuries.
Two
years ago, shortly after being elected to the Institute of Medicine
of the National Academy of Sciences, Kellermann was selected
to co-chair a committee analyzing the issues raised by the uninsured.
He was shocked by the committee’s findings.
“More
than 40 million Americans suffer the consequences of lacking
health insurance, but the crisis is threatening access to care
for 290 million Americans–all of us,” he says. “We
share a common destiny.”
The current overcrowding crisis is not caused by uninsured patients
using E.R.s inappropriately for minor problems, Kellermann says.
“That is a widespread and cruel misconception. Overcrowding
occurs when seriously ill and injured patients–victims
of car crashes, strokes, heart attacks, stabbings, and other
serious health problems–require hospitalization yet cannot
be moved to an inpatient unit because no beds are available.
And more patients are coming in every hour.”
Emergency room overcrowding is a life-or-death issue for everyone,
no matter how rich or well insured, Kellermann warns. “The
next time you have a crushing chest pain and are diverted because
the E.R. is full, money won’t make a bit of difference
because the system doesn’t have the capacity to care for
you,” he says.
Kellermann
has several ideas for improving the system: Place a few stretchers
in the hallways of each inpatient unit to spread the E.R.’s
burden. Put limits on the length of time admitted patients can
be held in the E.R. before being transferred. Provide financial
incentives to hospitals to keep E.R.s open and operating efficiently.
And devote a fair share of federal and state dollars to emergency
departments. “This is the biggest health threat facing
the middle class,” he says, “but the middle class
doesn’t know it.”